Know the Facts about Substance Use Disorder
 Substance Use Disorder Affects All Hoosiers
Substance Use Disorder Affects All Hoosiers
Every community in our state is touched by substance use disorder. Around half a million Hoosiers, or one in twelve of us1, meet the criteria for substance use disorder. You likely have a friend, family member, neighbor, or colleague who suffers from the disease of addiction.
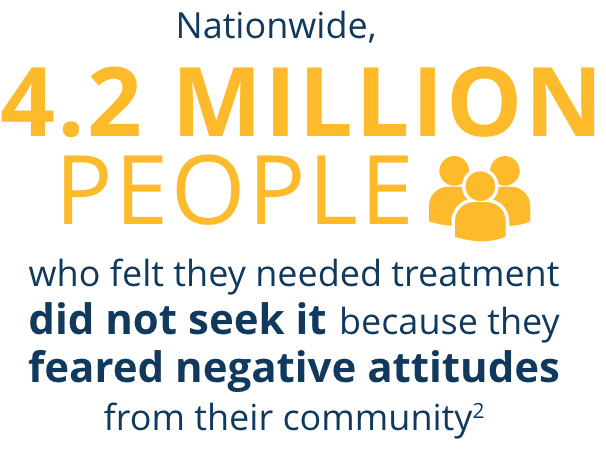
 Say No to Stigma
Say No to Stigma
Substance use disorder is a treatable disease, yet studies show that people who have it often face stigma and negative attitudes. They may encounter mistreatment, stereotyping, and negative bias from society, even in healthcare settings. These challenges can keep them from getting the help they need.
 See Beyond the Addiction
See Beyond the Addiction
We can fight against stigma in our own communities by supporting, listening to, and learning from those who live with substance use disorder. Destigmatizing this disease can help more Hoosiers get the treatment they need and ultimately find recovery.
How Will You See Me?
GRANDSON | SON | EMPLOYEE | MENTOR | FATHER | HUSBAND
And I have a substance use disorder. In other words, I’m living in recovery with an addiction disease. And now that you know, will you let it change how you see me? It’s OK to see my addiction, but I want you to know: it’s people choosing to see me as a person that changed my life.
How You Can Help
We can all play a part in helping Hoosiers affected by substance use disorders, from changing how we talk about addiction to supporting those in recovery.
![]()
Outreach Materials
We've compiled a set of materials to support our community partners in the fight against substance use disorder in Indiana and reducing stigma surrounding the disease.
Many of the photos included on this webpage are stock or original photography featuring paid actors. These photos do not represent individuals suffering from substance use disorder or living in recovery. The exception to this are photos of people who are named and share their personal story about substance use disorder. We are grateful for these brave survivors' willingness to come forward to help reduce the stigma of substance use disorder and provide encouragement for those suffering from this chronic disease.
1. Indiana University. The Crisis in Indiana: Addiction affects every aspect of Hoosier life. Publishing date not specified.
2. SAMHSA. Key Substance Use and Mental Health Indicators in the United States: Results from the 2021 National Survey on Drug Use and Health. Published December 2022.