Harm Reduction
Naloxone
Naloxone, also known by the brand name Narcan®, is a drug that can reverse the effect of an opioid or heroin overdose, and can be life-saving if administered in time. Naloxone can be given to anyone with symptoms of an opioid overdose.
- Distribution Program
- Naloxone 101
- Training Opportunities
- Resource Guide
- Administration Heat Map
- Syringe Services Schedule
Naloxone distribution program: Local health departments
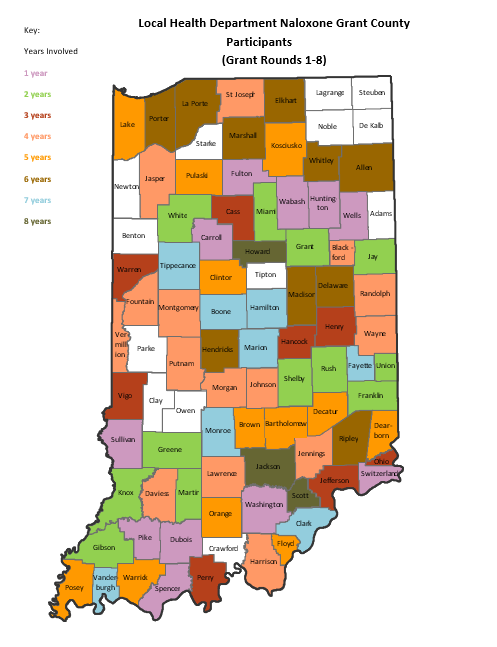
To increase the amount of naloxone available in communities across Indiana, the Indiana Department of Health (IDOH) has used state and federal funds to provide naloxone to local health departments (LHDs). IDOH has generated several grant opportunities for its naloxone distribution program, in which LHDs were awarded and responsible for distributing the free doses and providing naloxone training within their communities. As of July 2021, six rounds of the distribution program have been completed, with a seventh round in progress. In its first round, the program distributed 3,473 doses of naloxone to 23 LHD participants. Since then, the program has distributed a total of 98,239 doses of naloxone to LHDs with round 6 having the largest number of participants at 54 and round 7 having the largest number of doses distributed at 27,644 (and still growing). The map below shows each county that has been involved in the program, color coded by how many rounds they have been involved. Since 2018, approximately 4.2 million dollars has been spent for the LHDs. Each year the amount of money spent on doses increases, as the need for doses also increases. Approximately $860,000 was spent on kits in the entirety of the 2018 calendar year, while approximately $1,400,000 has been spent in only half of the 2021 calendar year.
If you are interested in learning more about the current grant opportunity, you may visit:
If you are a lay responder, i.e. a non-medical personnel who acts in an emergency, and would like to find out where to get naloxone naloxone, please visit optin.IN.gov and type in your zip code to find an entity near you.
Naloxone distribution program: First responders
To complement the distribution program, IDOH is targeting 49 rural counties that represent 1.47 million Indiana residents (22.3% of the total population). These counties have high rates of non-fatal emergency department visits due to opioid overdose and a lower reported use of naloxone by first responders. As part of this effort, the IDOH is also expanding the Indiana Recovery and Peer Support Initiative for referral to treatment.
Since the opening of the grant opportunity, 449 first responder agencies serving 45 rural counties were awarded a total of around 16,000 naloxone kits. Several more grant rounds will be opened in the future. Training is also offered for grantees through IDOH.
The 49 rural counties that are eligible to receive naloxone kits are listed below.
Adams | Blackford | Cass | Clinton | Crawford |
Daviess | Decatur | DeKalb | Dubois | Fayette |
Fountain | Franklin | Fulton | Gibson | Grant |
Greene | Henry | Huntington | Jackson | Jay |
Jefferson | Jennings | Knox | Kosciusko | Lagrange |
Lawrence | Marshall | Martin | Miami | Montgomery |
Noble | Orange | Parke | Perry | Pike |
Pulaski | Randolph | Ripley | Rush | Spencer |
Starke | Steuben | Switzerland | Tipton | Wabash |
Warren | Wayne | White | Union |
Trainings
IDOH has provided many local health departments in Indiana with naloxone rescue kits and training. If you would like more information regarding access to FREE training and kits in your county, contact your local health department or the Naloxone Program Manager.
Contact Information:
Laura Hollowell
Naloxone Program Manager, Division of Trauma and Injury Prevention
LHollowell@health.in.gov
Naloxone 101
- Naloxone, also known by the brand name Narcan®, is a non-narcotic that is an antidote for opioid overdoses. If administered in a timely manner, naloxone can reverse the life-threatening respiratory failure that is usually the cause of overdose deaths. Naloxone has been proven effective in reversing overdoses caused by heroin and prescription medications such as OxyContin, Percocet, Methadone and Vicodin.
- You may find a location by looking at this map, https://optin.in.gov/. No prescription is needed. A person seeking naloxone can ask the entity to use the state health commissioner’s statewide standing order.
- Ideally, naloxone should be kept between 40° F and 80° F (5° C to 25° C) in a dark, dry place. Naloxone is sensitive to temperature, and prolonged storage at temperatures above or below those recommended by the manufacturer may decrease the effectiveness of the drug. If your naloxone is left in freezing temperatures, make sure you hold it in a warm hand to thaw it prior to using it. Naloxone stored at high temperatures may lose some of its effectiveness but can still be used in an emergency.
- Yes, call an ambulance immediately after you have administered the naloxone. Give rescue breaths and start CPR, if you know how, until the person is breathing on his or her own. Position the person on his or her side in the recovery position once breathing has resumed. If there is no response to the first dose, give a second dose. Tell the people in the ambulance that you gave naloxone and at what time and show them the dose.
- No. Naloxone will not affect someone who has not ingested opioids.
- Individuals who are using opioids may experience withdrawal symptoms such as nausea, vomiting, confusion, agitation or combativeness when given naloxone. Naloxone is not an opioid or a controlled substance and has no potential for abuse. Allergic reactions to naloxone have been reported but are extremely rare.
- Naloxone has a shelf life of about two years. Make sure you check the expiration date listed on your naloxone and replace it if it has expired. If you are responding to an overdose and you notice that your naloxone has expired, you can still use it. Expired naloxone may still be effective enough to save a life and it will not hurt anyone if you use it.
Contact Information:
Laura Hollowell
Naloxone Program Manager
LHollowell@health.in.gov
Naloxone Training Opportunities
IDOH – Provides trainings to rural first responder agencies and the general public upon request.
The Indiana Department of Health (IDOH) is pleased to offer virtual naloxone administration trainings that are free and self-paced. These courses cover topics such as Indiana overdose statistics, stigma reduction, naloxone administration, and treatment options for substance use disorder.
IDOH is offering three online courses available on the Indiana TRAIN platform:
- Naloxone Administration Training: First Responders: ID 1122357
- Naloxone Administration Training: First Responder Refresher: ID 1122441
- Naloxone Administration Training: Public: ID 1122355
For more information about accessing these training opportunities, check out our training guide.
OptIN – Provides a list of entities that are naloxone providers.
Overdose Lifeline- Conducts community-based trainings.
Bitter Pill – Naloxone training resources.
Indiana Recovery Alliance – Distributes naloxone during daily outreach and through community trainings. The Monroe County Health Department offers naloxone through community trainings to the public as well as providing naloxone to emergency responders such as local fire departments, local police departments, community justice and local emergency departments.
IDOH has provided many local health departments in Indiana with naloxone rescue kits and training. If you would like more information regarding access to FREE training and kits in your county, contact your local health department or the Naloxone Program Manager.
Contact Information:
Laura Hollowell
Naloxone Program Manager
LHollowell@health.in.gov
Naloxone Resource Guide for Local Health Departments
This resource guide was created by the Indiana State Department of Health (IDOH) Division of Trauma and Injury Prevention as a resource for local health departments (LHDs) who have been awarded the Naloxone Rescue Kit Grant by IDOH. The guide aims to provide guidance for LHDs to successfully distribute naloxone kits to high-need individuals in their counties. A special thank you goes to staff from the Hamilton, Hendricks and Howard county health departments for helping to compile this guide.
Services co-offered with naloxone training
Local health departments are required to offer a number of resources and services when providing naloxone training to laypersons (I.C. 16-42-27). This includes education on how to administer naloxone and a list of drug addiction treatment resources, such as centers that offer medication assisted treatment and referrals to these facilities. In addition, LHDs are encouraged, though not required, to provide a variety of other resources to trainees. Some of these resources can include:
Educational resources
- Important information about naloxone that includes signs and symptoms of an opioid overdose
- Educational sheet about common opioid drugs that also describes signs and symptoms of an opioid overdose
- FAQs about syringe exchange and harm reduction programs
- Syringe service fact sheet
- Pamphlet about commonly abused drugs (great for school staff)
- Naloxone myths debunked fact sheet
- What parents need to know fact sheet
- The Harm Reduction Coalition’s overdose prevention resource page
- Check out the printable resources page for more fact sheets
Services offered
- List of treatment resources in LHD county (required)
- The Indiana Criminal Justice Institute and the Indiana State Police have compiled a list of treatment centers
- Substance Abuse and Mental Health Services Administration (SAMHSA) has created a search engine that allows users to type in a zip code and find nearby treatment centers
- Family and Social Services Administration (FSSA) has compiled a list of Community Mental Health Centers in Central Indiana
- IDOH has compiled a list Treatment Centers (residential and outpatient)
- The Hendricks County Health Partnership and the Hendricks County Health Department have compiled the Central Indiana Substance Abuse Treatment Resource Guide
- List of other naloxone providers in the county (check optIN)
- Information about unused drug disposal in the county
- Referrals to the local Parents of Addicted Loved Ones
- Information about syringe exchange programs and safe sharps disposal in the county and surrounding counties
- Information about STD testing in the county
- Information about HIV and Hepatitis C testing in the county
- Information about the immunization clinic in the LHD (if those services are offered)
- Support for family members through education materials and referrals to local community resources
- CPR training may be offered in addition to naloxone training
Other
- Heart health and the opioid epidemic from the American Heart Association
Stakeholder partnerships
To best combat the opioid epidemic, partnerships need to be formed among a variety of stakeholders. This applies to the naloxone distribution program as well, where collaborating with different community partners can help make the distribution program a success. Below is a list of agencies that local health departments can provide with naloxone to use in case of an emergency. These agencies can also provide naloxone kits to community members and help spread the word about the program.
- Local clinics and primary care practices
- Local hospitals (especially emergency departments)
- Health department’s nursing clinic
- Syringe Services Program in the community
- Substance abuse and counseling centers
- Substance abuse work groups (if such groups exist)
- Schools (train school nurses, administrators and maintenance staff)
- Law enforcement
- Fire departments
- EMS (provide naloxone training to EMS staff and/or solicit information as to where they frequently encounter opioid overdoses so you can target those areas)
- Local libraries
- Overdose Lifeline
- Any other agency or organization that works with high-risk individuals
Ways to spread the word about the naloxone program
Below is a list of potential outreach methods local health departments can employ to spread the news about the naloxone distribution program.
Create flyers advertising the naloxone distribution program. A sample copy of such a flyer is located here (courtesy of Howard County Health Department). Flyers can be distributed in:
- Substance abuse treatment centers
- Offices of mental health service providers
- Food pantries
- Primary care physician clinics
- Clinics that provide free health services
- Gas stations
- Motels
- Schools (the best initial point of contact will likely be a school nurse)
- Shelters
- Local government agencies (transportation office, social services office, etc.)
- Any other agency or not-for-profit that works with high-risk individuals
- Develop small cards with contact information for the naloxone distribution program. The Howard County Health Department uses brightly colored cards that are the size of business cards
- Partner with the community drug task force (if one exists) or the local coordinating committee and ask them to distribute flyers and spread the word
- Set up focus groups with recently-released inmates to determine the best paths for reaching out to members of the community who are at risk or connected to someone at risk
- Post on social media, including Twitter, Facebook and Instagram
- Contact local news stations, radio stations and newspapers and ask them to do a story on the program
- Indiana 211 – ensure that your health department is listed on their website as offering free naloxone training and kits
- Update the health department’s website to include information about this program. Encourage partners in your communities to include information on their websites as well (including law enforcement agencies)
- Word of mouth – encourage community members who come in for a naloxone training to let their contacts know about the program. This can also be accomplished by speaking at community meetings/events
- Nextdoor app – a free, private social network that serves as a popular way for people to find out what is happening in their local communities
- Send e-mails to your listserv if you have one
- Ask other agencies and organizations in the county to send out e-mails to their listserv as well
- Set up a booth at community events, which could include town hall meetings, conferences, school events and others
Other useful resources for the naloxone distribution program
Consent form – Create a consent form that all laypersons can sign before receiving a naloxone training and kit. Here is a sample consent form, courtesy of the Hendricks County Health Department.
Flyers – Create flyers to advertise your naloxone distribution program. Sample copies of such flyers are located here (courtesy of Howard County Health Department) and here (courtesy of Hendricks County Health Department).
Policies and procedures – Create an internal document that outlines the policies and procedures set forth by your health department regarding the naloxone distribution program.
- Hendricks County Health Department has provided a copy of its policies and procedures. This document lays out the procedure for who is allowed to train laypersons and how they are to proceed with training (both in an individual and group setting)
- Howard County Health Department has also provided a copy of their policies and procedures, which outlines how the naloxone training should proceed
Kit stickers – When putting together naloxone kits, it is useful to have these stickers on the kit to remind laypersons that they are required to call 911 either immediately before or after administering naloxone per I.C. 16-42-27 and to remind them to fill out the pre- and post- cards.
Educational document about the program - The Hendricks County Health Department created a document explaining the naloxone distribution program, specifically written for agencies and businesses inquiring about the program. Feel free to edit and customize it as needed.
Educational document for schools - The Hendricks County Health Department created a document that explains why naloxone is important in schools. You can use this document to get the school officials in your county on board with your naloxone distribution program.
A reminder about requirements
As a reminder, LHDs that have been awarded the naloxone distribution grant are required to do the following:
- Must provide adequate education when distributing naloxone kits in a manner consistent with I.C. 16-42-27 and provide documentation thereof
- Must provide treatment program contact information for the community when distributing naloxone kits
- Must register with optIN
- If the awardee’s point-of-contact changes anytime during the naloxone kit distribution or reporting period, the awardee must notify the IDOH within five business days after the change and provide the contact information for the new contact
- Must not charge the recipients of the naloxone kits and must ensure that naloxone kits are not resold after distribution
- Must submit scheduled reports. If you need help filling out the report, please contact IDOH's Naloxone Program Manager.
Contact Information:
Laura Hollowell
Naloxone Program Manager
LHollowell@health.in.gov
Naloxone Administration Heat Map
This tool from Next Level Recovery website provides insight into the incident location where naloxone was administered and reported by EMS providers throughout the state of Indiana. Indiana EMS providers report locations of patient encounters during which naloxone was administered when an opioid overdose was suspected. The drug, also known by the brand name Narcan®, reverses the effects of an opioid overdose and is administered with the intent to save the life of the patient. The Naloxone Administration Heat Map shows naloxone administrations as reported by EMS provider agencies since January 1, 2014.
For more information or to access this interactive map, click on the photo below:
Syringe Services Schedule
Provides new/sterile syringes, sharps disposal containers, free HIV and hepatitis C testing, referrals to treatment and other social services (medical, food, housing etc.).
All days and hours of operation are subject to change based upon local decision. Verify operation times directly with them.
Allen
- 4817 New Haven Avenue, Fort Wayne, IN 46803
-Tuesdays from 1 p.m. to 3:30 p.m. (Fixed)
Clark
- Clark County HD, 1201 Wall Street, Jeffersonville, IN 47130
-Mondays through Fridays from 9 a.m. to 3 p.m. (Fixed)
Fayette
- Connection Café, 635 N Central Ave, Connersville, IN 47331
-Thursdays from 9 a.m. to 7 p.m. (Fixed)
-Fridays & Saturdays from 4 p.m. to 10 p.m. (Fixed)
Madison-Aspire
- 2009 Brown Street, Anderson, IN 46016
-Mondays & Wednesdays from 11 a.m. to 5 p.m. (Fixed)
- 10731 SR 13, Elwood, IN 46036
-Thursdays from 1p.m. to 4 p.m. (Mobile Unit)
Marion
- 7551 Shelby St, Indianapolis, IN 46227
-Mondays from 12:30 p.m. to 3 p.m. (Fixed)
- Damien Center, 1416 E Washington St, Indianapolis, IN 46201
-Wednesdays from 2 p.m. to 6 p.m. (Mobile Unit)
- 1035 N Olney St, Indianapolis, IN 46201
-Fridays from 11 a.m. to 3 p.m. (Mobile Unit)
Monroe-IRA
- Shalom Community Center, 620 S. Walnut St, Bloomington, IN 47401
-Mondays & Fridays from 12 p.m. to 2 p.m. (Mobile Unit)
- Office Indiana Recovery Alliance, 118 S. Rogers St, Bloomington, IN 47404
-Tuesdays, Thursdays, Saturdays, & Sundays from 5 p.m. to 7 p.m. (Fixed)
Tippecanoe
- Lafayette Transitional Housing Center (LTHC), 815 N 12th St, Lafayette, IN 47904
-Tuesdays from 3 p.m. to 6 p.m. (Fixed)
-Wednesdays from 2 p.m. to 4 p.m. (Fixed)
-Fridays from 1 p.m. to 5 p.m. (Fixed)
-Saturdays from 10 a.m. to 1 p.m. on the 1st and 3rd Saturdays of each month. (Fixed)
Wayne
- Wayne County HD, 100 S. 5th St, Richmond, IN 47374
-Tuesdays from 12 p.m. to 2 p.m. (Fixed)
- Restoration Outreach Centre (ROC), 310 N. 19th St, Richmond, IN 47374
-Tuesdays from 3 p.m. to 4:30 p.m. (Fixed)
- Centerstone, 100 N. 15th St, Richmond, IN 47374
-Thursdays from 3 p.m. to 4:30 p.m. (Fixed)
OptIN
Save a Life. Help prevent overdose deaths.