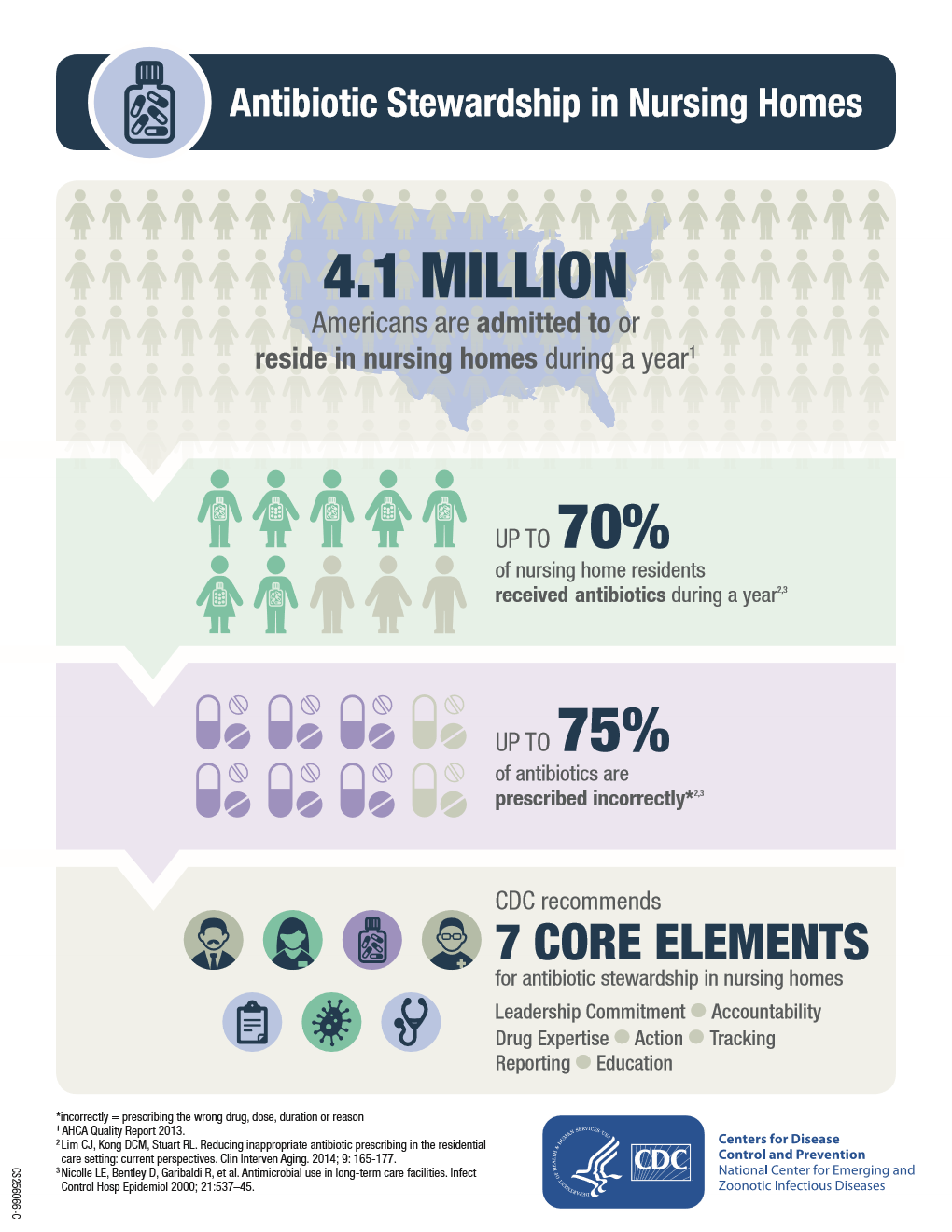
Antibiotics are among the most frequently prescribed medications in nursing homes, with up to 70% of residents receiving one or more courses of systemic antibiotics in a year. Harms from overuse are significant for older adults receiving care in nursing homes. Improving the use of antimicrobials in healthcare is an important public health issue as well as a national priority. A growing body of evidence demonstrates that Antimicrobial Stewardship Programs can optimize the treatment of infections and reduce adverse events associated with antibiotic use, such as Clostridioides difficile infection.
In 2015, the Centers for Disease Control and Prevention (CDC) published The Core Elements of Antibiotic Stewardship for Nursing Homes. This document adapts the core elements of hospital antibiotic stewardship into practical strategies for implementation in the uniquely different long-term care setting.
- Leadership Commitment: Demonstrate support and commitment to safe and appropriate antibiotic use in your facility
- Accountability: Identify physician, nursing, and pharmacy leads responsible for promoting and overseeing antibiotic stewardship activities in your facility
- Drug Expertise: Establish access to consultant pharmacists or other individuals with experience or training in antibiotic stewardship for your facility
- Action: Implement at least one policy or practice to improve antibiotic use
- Tracking: Monitor at least one process measure of antibiotic use and at least one outcome from antibiotic use in your facility
- Reporting: Provide regular feedback on antibiotic use and resistance to prescribing clinicians, nursing staff and other relevant staff
- Education: Provide resources to clinicians, nursing staff, residents and families about antibiotic resistance and opportunities for improving antibiotic use
Page last reviewed and updated: October 2024